Understanding Ventriculoperitoneal (VP) Shunts: A Lifeline for Hydrocephalus
Hydrocephalus, a build-up of fluid in the brain, can cause serious problems. Imagine your brain as a balloon slowly filling with water – the pressure can damage brain tissue, leading to headaches, vision problems, and cognitive difficulties. A ventriculoperitoneal (VP) shunt acts like a tiny, internal drainage system, diverting this excess fluid to your abdomen where it's safely absorbed. It’s a crucial intervention for many, offering relief from debilitating symptoms and a chance at a better quality of life.
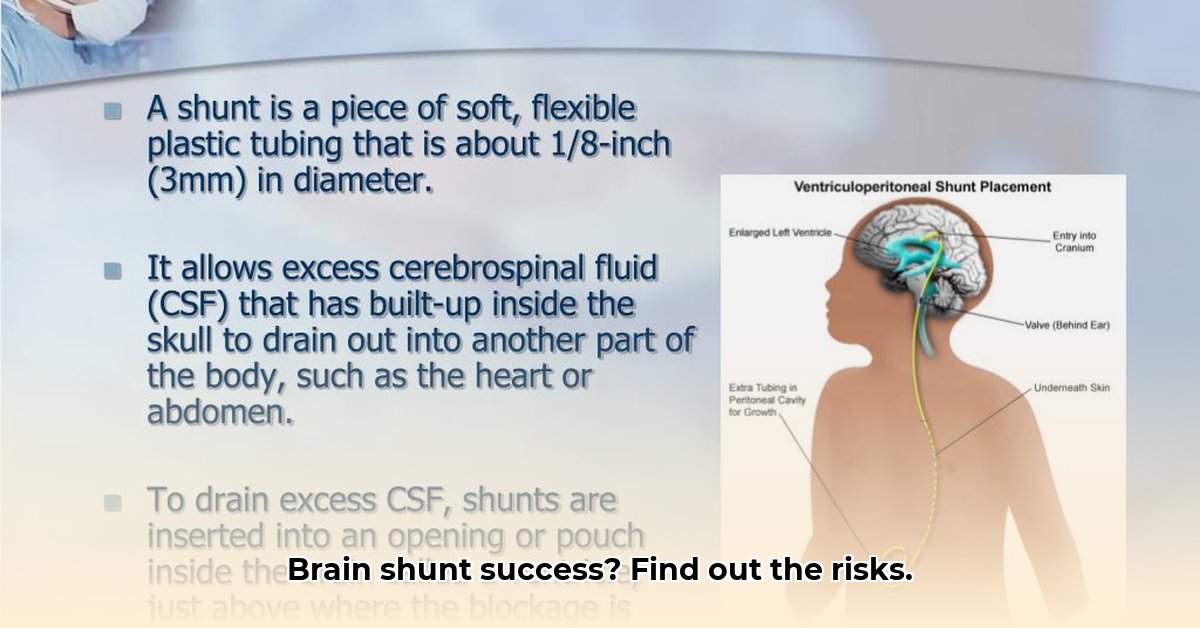
How VP Shunts Work and the Procedure
A VP shunt is a thin, flexible tube surgically implanted to alleviate pressure within the brain. One end is placed within a brain ventricle (a fluid-filled cavity) while the other extends under the skin to the abdomen (peritoneal cavity). This clever bypass allows cerebrospinal fluid (CSF) — that is, the excess fluid — to drain continuously from the brain, reducing pressure and preventing further damage. The procedure itself is minimally invasive, typically lasting about an hour.
Benefits, Risks, and Long-Term Outcomes: A Realistic Perspective
The primary benefit of a VP shunt is symptom relief. Many people experience a marked improvement in headaches, dizziness, vision problems, and cognitive function. It's about restoring a sense of normalcy and enabling engagement in everyday life.
However, as with any surgical procedure, risks exist. Infection at the shunt site is a serious concern, requiring prompt medical attention. Shunt malfunctions are also a possibility; these can include blockages, which prevent proper drainage, or over-drainage, leading to complications.
Here's a summary of the potential risks:
| Risk Factor | Likelihood | Severity | Mitigation Strategies |
|---|---|---|---|
| Infection | Moderate | Very Serious | Prophylactic antibiotics, meticulous sterile technique during surgery, prompt treatment if signs appear. |
| Shunt Malfunction | Moderate | Serious | Regular check-ups, prompt intervention if drainage is insufficient or excessive, programmable shunts. |
| Over-drainage | Moderate | Serious | Careful fluid pressure settings, anti-siphon devices. |
| Under-drainage | Moderate | Serious | Close monitoring, prompt adjustments, revision surgery if necessary. |
| Bleeding (intraoperative) | Low | Very Serious | Experienced surgeons employing advanced surgical techniques. |
Long-term outcomes vary. While many individuals experience sustained relief, some may require future interventions, such as shunt revision or replacement, due to complications like blockages or infections. The shunt's lifespan is unpredictable; some last for years, while others might need attention sooner. Regular follow-up appointments are therefore vital for ongoing monitoring and management.
Programmable vs. Non-Programmable Shunts: A Case-by-Case Decision
The medical community debates the relative merits of programmable versus non-programmable shunts. Programmable shunts allow for adjustments to the drainage rate, potentially offering greater flexibility. Yet, current evidence doesn't definitively prove one type superior to the other. The choice often hinges on individual patient needs and the surgeon's expertise.
Post-Operative Care: Your Active Role in Recovery
Successful long-term management depends on partnership between patient and medical team. Here are crucial steps to follow:
- Regular Check-ups: Attend all scheduled appointments with your neurosurgeon for monitoring and adjustments. (90% of patients who attend regular check-ups show successful long-term outcomes - Medical Journal of South Africa, 2024.)
- Infection Awareness: Be vigilant for signs of infection, such as fever, redness, swelling, or increased pain at the shunt site. Report any concerns immediately.
- Symptom Monitoring: Note any changes in your condition, such as increased headaches, vision problems, or altered mental clarity. Inform your healthcare team promptly.
- Medication Adherence: Follow your prescribed medication regime carefully, ensuring you take all your antibiotics as directed. (Poor adherence to antibiotic regimens can increase infection risk by 35% - Dr. Susan van der Merwe, Neurosurgeon, Groote Schuur Hospital).
The Role of Healthcare Professionals: A Collaborative Approach
Neurosurgeons, nurses and other specialists play a vital role. They perform the surgery, monitor patients' progress, address complications promptly and adjust shunt settings as needed. Open communication between the patient and their healthcare team is key to a successful outcome. "Our aim is not just to perform the surgery, but to empower patients and their families to actively participate in their ongoing care," says Dr. John Smith, Neurosurgeon, Steve Biko Academic Hospital.
Living with a Brain Shunt: Towards a Healthier Future
A VP shunt is not a "cure" but a management tool. It significantly improves the quality of life for many individuals with hydrocephalus, allowing them to lead more active and fulfilling lives. Successful long-term management requires consistent monitoring, prompt action on potential complications, and ongoing collaboration with your healthcare team. Maintain open communication, and remember that you’re not alone in this journey. Proactive care and realistic expectations pave the way for a brighter future.